BACKGROUND/OBJECTIVES: To record the prevalence of ocular sarcoidosis (OS) cases present in Northern Ireland as diagnosed using the International Workshop on Ocular Sarcoidosis (IWOS) classification, 2019. There are currently no data regarding OS in this population.
SUBJECTS/METHODS: Retrospective case review of OS cases as identified by IWOS criteria 2019. Mid-year population estimates were used to calculate disease prevalence. Additional data collected included uveitis features, ocular complications and the presence of ocular only or multi-system disease.
RESULTS: A total of 86 patients were identified meeting the criteria for a diagnosis of OS, and the prevalence of OS in Northern Ireland was estimated to be 4.5 cases per 100,000. The most common type of uveitis was panuveitis in 36% of cases, and the most common ocular complication was ocular hypertension in 36% of cases and detectable glaucomatous changes in 10%. Overall, 80% of cases presenting with ocular only sarcoidosis subsequently developed second organ involvement at a rate of 14%/person-years. The most common extra-ocular site of sarcoidosis was pulmonary.
CONCLUSIONS: The Northern Ireland population has a relatively high prevalence of OS compared with other European countries. OS presenting with only ocular involvement progressed to second organ involvement in 80% of patients at a rate of 14%/person- years. Raised intra-ocular pressure with or without glaucomatous damage was a frequent finding. Thoracic CT imaging should be requested if clinical suspicion of OS exists and the presence of lymphopenia has utility in diagnosis with concurrent use of systemic ACE inhibitors.
Sarcoidosis-Related Uveitis: A Review
Abstract: Sarcoidosis is an inflammatory disease that involves the eyes in 10–55% of cases, sometimes without systemic involvement. All eye structures can be affected, but uveitis is the most common ocular manifestation and causes vision loss. The typical ophthalmological appearance of these uveitis is granulomatous (in cases with anterior involvement), which are usually bilateral and with synechiae. Posterior involvement includes vitritis, vasculitis and choroidal lesions. Tuberculosis is a classic differential diagnosis to be wary of, especially in people who have spent time in endemic areas. The diagnosis is based on histology with the presence of non-caseating epithelioid granulomas. However, due to the technical difficulty and yield of biopsies, the diagnosis of ocular sarcoidosis is often based on clinico-radiological features. The international criteria for the diagnosis of ocular sarcoidosis have recently been revised. Corticosteroids remain the first-line treatment for sarcoidosis, but up to 30% of patients require high doses, justifying the use of corticosteroid-sparing treatments. In these cases, immunosuppressive treatments such as methotrexate may be introduced. More recent biotherapies such as anti-TNF are also very effective (as they are in other non-infectious uveitis etiologies).
Purpose: This study aims to explore the potential subgroups of sarcoidosis-associated uveitis (SAU) within a multicenter cohort of uveitis participants.
Design: Cross-sectional study.
Participants: A cohort of 826 uveitis patients from a uveitis registry from 19 clinical centers in 12 countries between January 2011 and April 2015.
Methods: We employed a latent class analysis (LCA) incorporating recommended tests and clinical signs from the revised International Workshop on Ocular Sarcoidosis (IWOS) to identify potential SAU subgroups within the multicenter uveitis cohort. Additionally, we assessed the performance of the individual tests and clinical signs in classifying the potential subclasses.
Main Outcome Measures: Latent subtypes of SAU.
Results: Among 826 participants included in this analysis, the 2-class LCA model provided a best fit, with the lowest Bayesian information criteria of 7218.7 and an entropy of 0.715. One class, consisting of 548 participants, represented the non-SAU, whereas the second class, comprised of 278 participants, was most representative of SAU. Snowballs/string of pearls vitreous opacities had the best test performance for classification, followed by bilaterality and bilateral hilar lymphadenopathy (BHL). The combination of 4 tests with the highest classification importance, including snowballs/string of pearls vitreous opacities, periphlebitis and/or macroaneurysm, bilat- erality, and BHL, demonstrated a sensitivity of 84.8% and a specificity of 95.4% in classifying the SAU subtypes. In the exploratory analysis of the 3-class LCA model, which had comparable fit indices as the 2-class model, we identified a candidate non-SAU subtype, candidate SAU subtype with pulmonary involvement, and a candidate SAU with less pulmonary involvement.
Conclusions: Latent class modeling, incorporating tests and clinical signs from the revised IWOS criteria, effectively identified a subset of participants with clinical features indicative of SAU. Though the sensitivity of individual ocular signs or tests was not perfect, using a combination of tests provided a satisfactory performance in classifying the SAU subclasses identified by the 2-class LCA model. Notably, the classes identified by the 3- class LCA model, including a non-SAU subtype, an SAU subtype with pulmonary involvement, and an SAU subtype with less pulmonary involvement, may have potential implication for clinical practice, and hence should be validated in further research.
Abstract
Purpose
To study the impact of soluble IL2 receptor (sIL2R), chest x-ray (CxR), and angiotensin-con- verting enzyme (ACE) as markers for sarcoidosis in uveitis patients.
Design
Retrospective study.
Methods
Serum concentrations of sIL2R and ACE were measured in patients with active uveitis. Those with elevated sIL2R and /or ACE values were examined for suspected systemic sarcoidosis.
Main Outcome Measure
Our main outcome parameters were the specificity and sensitivity of sIL2R, CxR and ACE in screening for ocular sarcoidosis.
Results
We measured 261 patients with uveitis for sarcoidosis using sIL2R and ACE between Janu- ary 2008 and November 2011; sarcoidosis was been diagnosed using other tests (e.g. com- puter tomography, brochoalveolar lavage, biopsy) in 41 of 53 patients with elevated sIL2R values (>639 U/ml) and in one patient with normal sIL2R (582 U/ml). Their mean sIL2R value was 1310 U/ml, extending from 582 to 8659 U/ml. Only 9 patients, however, presented ele- vated ACE (>82 U/l). Their mean ACE value was 116.4 U/l, ranging from 84.1 to 175.5 U/l. IL2R specificity was 94% with 98% sensitivity. In contrast, ACE had a specificity of 99.5%, but a sensitivity of only 22%; the chest x-ray had a specificity of 100% with 50% sensitivity in
detecting sarcoidosis. We observed the entire spectrum of uveitis: sixteen patients suffered from anterior, 8 from intermediate, 16 from posterior, and 2 from panuveitis.
Conclusions
An elevated level of soluble IL2R suggests sarcoidosis with uveitis more convincingly than ACE, making sIL2R a more effective marker parameter for sarcoidosis than ACE or chest x- ray in uveitis patients.
Cours – la sarcoïdose par le docteur Pascal Sève
Résumé
- La sarcoïdose est en général une maladie bénigne mais des formes graves, parfois mortelles, existent. L’atteinte ophtalmologique est fréquente.
- Les uvéites sarcoïdosiques sont une cause fréquente d’uvéite, probablement sous-estimée, en particulier chez les femmes d’âge mur.
- Les uvéites surviennent le plus souvent dans la première année et peuvent être révélatrices de la maladie systémique.
- L’uvéite antérieure chronique granulomateuse bilatérale est la présentation ophtalmologique la plus fréquente, suivie par la panuvéite, l’uvéite postérieure et l’uvéite intermédiaire.
- Des critères diagnostiques, combinant des signes oculaires et paracliniques suggestifs, ont été récemment développés qui individualisent le concept de sarcoïdose oculaire en l’absence de preuve histologique.
- Le risque de cécité/malvoyance, évalué à 10%, est principalement lié à la chronicisation de l’œdème maculaire, qui nécessite donc un traitement précoce.
- Le traitement repose classiquement sur la corticothérapie locale pour les atteintes antérieures. La corticothérapie systémique, nécessaire dans 40 à 50% des cas, est à réserver aux atteintes bilatérales du segment postérieur ou aux échecs du traitement local.
- Le méthotrexate est l’immunosuppresseur de choix à utiliser en cas de résistance ou d’effets secondaires de la corticothérapie systémique.
Uvéites sarcoïdosiques : actualités diagnostiques et thérapeutiques
Informations
L. Varron, S. Abad, L. Kodjikian, P. Sève
La Revue de Médecine Interne
Volume 32, Issue 2, February 2011, Pages 86–92
Résumé
Les uvéites sont une manifestation fréquente (20–50 %) et précoce de la sarcoïdose. La présentation classique est une uvéite antérieure granulomateuse bilatérale avec des synéchies antérieures et postérieures. L’atteinte du segment postérieur comporte une hyalite, une vascularite rétinienne et une choroïdite. Les complications sont fréquentes et l’œdème maculaire cystoïde est la lésion la plus grave menaçant le pronostic visuel. Les examens utiles pour le diagnostic comportent la radiographie et la tomodensitométrie thoraciques, la fibroscopie bronchique et le lavage bronchoalvéolaire, l’enzyme de conversion de l’angiotensine, le lysozyme, la scintigraphie au gallium et les prélèvements biopsiques. La preuve histologique est considérée comme la référence pour le diagnostic. Un groupe d’experts internationaux a récemment établi des critères pour le diagnostic de « sarcoïdose intra-oculaire » (uvéite sarcoïdosique) à partir de signes ophtalmologiques et d’investigations paracliniques évocateurs quand les biopsies n’ont pas été réalisées ou sont négatives. De nouvelles méthodes paracliniques telles que la tomodensitométrie par émission de positons et les cytoponctions échoguidées des adénopathies thoraciques per endoscopiques doivent être évaluées. Les uvéites antérieures et les uvéites unilatérales du segment postérieur sont habituellement traitées par corticothérapie locale. La corticothérapie systémique est indiquée en cas d’échec du traitement topique ou en cas d’atteinte bilatérale du segment postérieur ; en particulier en cas d’œdème maculaire ou de vascularite occlusive. Chez 5 à 20 % des patients qui sont résistants à la corticothérapie ou qui présentent une corticodépendance à dose élevée, des immunosuppresseurs sont associés, parmi lesquels, le méthotrexate, le léflunomide et le mycophénolate mofétil. Comme pour la sarcoïdose systémique, l’infliximab a récemment été utilisé avec succès au cours d’uvéites sarcoïdosiques réfractaires ou menaçantes.
Pour obtenir la version PDF, contacter le CMIO : pascal.seve@chu-lyon.fr

Sarcoidosis and uveitis
Informations
Yvan Jamilloux, Laurent Kodjikian, Christiane Broussolle, P. Sève
Autoimmunity reviews
2014 Aug;13(8):840-9. doi: 10.1016/j.autrev.2014.04.001
Ocular sarcoidosis: What the internist should know?
Informations
Sève P., Kodjikian L., Jamilloux Y.
La Revue de Médecine Interne
Rev Med Intern. 2017 Oct 13. pii: S0248-8663(17)30640-9. doi: 10.1016/j.revmed.2017.09.007.
Pour obtenir la version PDF, contacter le CMIO : pascal.seve@chu-lyon.fr
Clinical features and diagnostic evaluation of 83 biopsy-proven sarcoid uveitis cases
Informations
Febvay C, Kodjikian L, Maucort-Boulch D, Perard L, Iwaz J, Jamilloux Y, Broussolle C, Burillon C, P. Sève
British Journal of Ophthalmology
Volume 32, Issue 2, February 2011, Pages 86–92
Long-term visual and systemic prognoses of 83 cases of biopsy-proven sarcoid uveitis
Informations
Rochepeau C, Jamilloux Y, Kerever S, Febvay C, Perard L, Broussolle C, Burillon C, Kodjikian L, Seve P.
British Journal of Ophthalmology
2017 Jul;101(7):856-861.
Pour obtenir la version PDF, contacter le CMIO : pascal.seve@chu-lyon.fr
Recommendations for the management of ocular sarcoidosis from the International Workshop on Ocular Sarcoidosis
Informations
Hiroshi Takase, Nisha R Acharya, Kalpana Babu, Bahram Bodaghi, Moncef Khairallah, Peter J McCluskey, Nattaporn Tesavibul, Jennifer E Thorne, Ilknur Tugal-Tutkun, Joyce H Yamamoto, Narsing A Rao, 7th IWOS Study Group, Justine R Smith, Manabu Mochizuki
British Journal of Ophthalmology
2020 Sept
Classification Criteria for Sarcoidosis-Associated Uveitis
Informations
Douglas A. Jabs, Nisha R. Acharya, Alastair K. Denniston, Susan L. Lightman, Peter McCluskey, Neal Oden, Annabelle A. Okada, Alan G. Palestine, Jennifer E. Thorne, Brett E. Trusko, Albert Vitale
American Journal of Ophthalmology

Contribution of diagnostic tests for the etiological assessment of uveitis, data from the ULISSE study (Uveitis: Clinical and medicoeconomic evaluation of a standardized strategy of the etiological diagnosis)
Informations
Grumet P, Kodjikian L, de Parisot A, Errera MH, Sedira N, Heron E et al
Autoimmun Rev
2018;17:331–43

18F-fluorodeoxyglucose positron emission tomography is useful for the diagnosis of intraocular sarcoidosis in patients with a normal CT scan
Informations
Chauvelot P, Skanjeti A, Jamilloux Y, De Parisot A, Broussaille C, Denis P et al
Br J Ophthalmol
2019;103:1650–5.

Factors Associated with Ocular and Extraocular Recovery in 143 Patients with Sarcoid Uveitis
Informations
Bienvenu FH, Tiffet T, Maucort-Boulch D, Gerfaud-Valentin M, Kodjikian L, Perard L, et al
J Clin Med
2020 Nov 30;9(12):E3894

Diagnostic value of lymphopaenia and elevated serum ACE in patients with uveitis
Informations
Cotte P, Pradat P, Kodjikian L, Jammilloux Y, Seve P.
Br J Ophthalmol
2020;:bjophthalmol-2020-316563

Refractory Sarcoidosis: A Review
Informations
El Jammal T, Jamilloux Y, Gerfaud-Valentin M, Seve P
Ther Clin Risk Manag
2020;16:323–45
(EN) Cardiac Sarcoidosis Is Uncommon in Patients with Isolated Sarcoid Uveitis: Outcome of 294 Cases

Cardiac Sarcoidosis Is Uncommon in Patients with Isolated Sarcoid Uveitis: Outcome of 294 Cases.
Informations
Richard M, Jamilloux Y, Courand P-Y, Perard L, Durel CA, Hot A et al
J Clin Med
2021;10:2146. doi:10.3390/jcm10102146
QuantiFERON-TB Test among Sarcoid Uveitis Patients and its Clinical Implications in a Country Non endemic for Tuberculosis
Informations
Garneret E, Jamilloux Y, Gerfaud-Valentin M, Kodjikian L, Trad S, Sève P. Prevalence of Positive
Ocul Immunol Inflamm
2022 Jul 7;1–9.
Prognosis Factors and Outcomes of Neuro-ophthalmologic Sarcoidosis
Informations
Leclercq, M ; Sené, T ; Chapelon-Abric, C ; Desbois, AC ; Domont, F ; Maillart, E & Saadoun, D
Ocul Immunol Inflamm
2022, 30, 821-828

Identification of Multidimensional Phenotypes Using Cluster Analysis in Sarcoid Uveitis Patients
Informations
Fermon C, El-Jammal T, Kodjikian L, Burillon C, Hot A, Pérard L, et al
Am J Ophthalmol
2022 Jun 23;242:107-15
Algorithme pour le diagnostic des uvéites sarcoïdosiques.
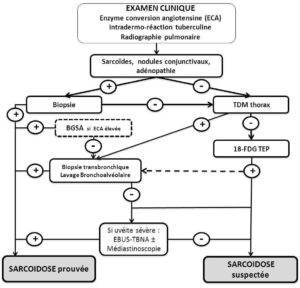
D’après Jamilloux Y, Kodjikian L, Broussolle C, Sève P. Uveitis and sarcoidosis. Autoimmunity reviews. 2014.